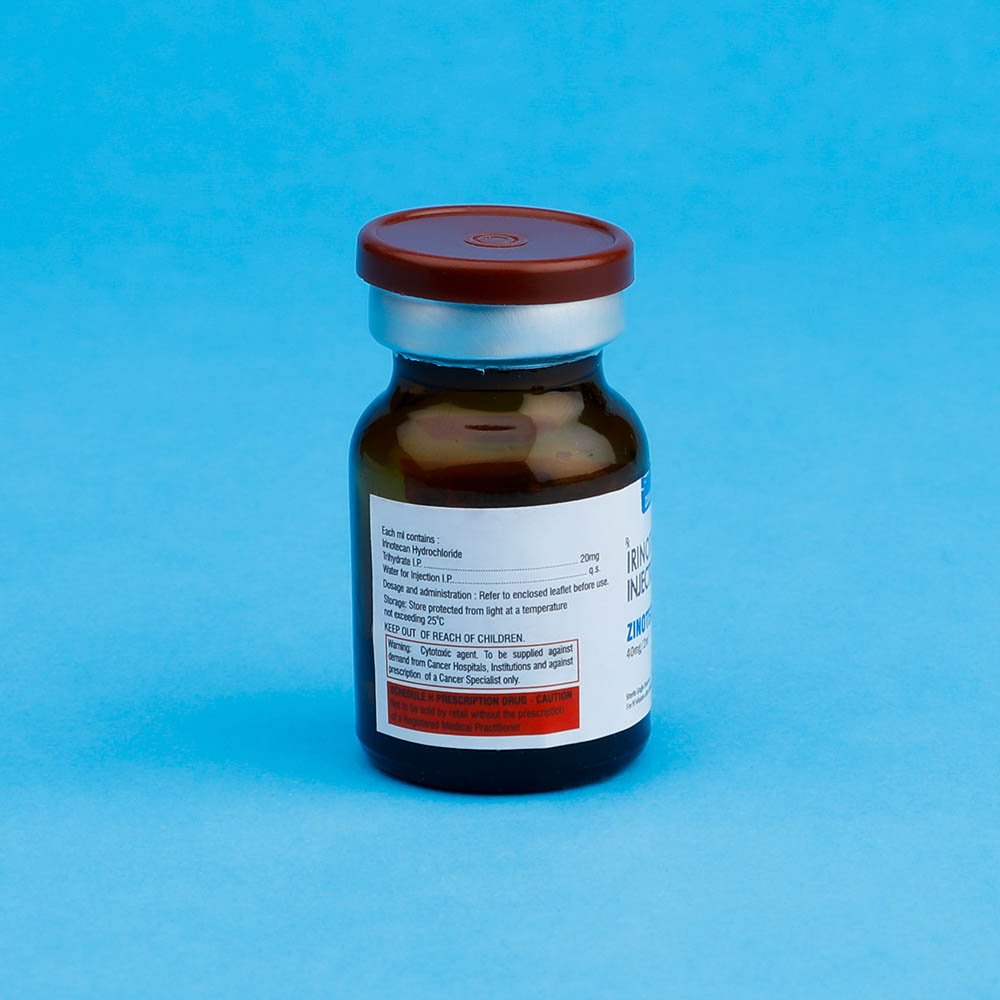
Zinotecan- Irinotecan Inj
Irinotecan Inj
Strength: 40MG, 100MG
Pack Size: 1 vial
Drug Class: Antineoplastic and immunomodulating agents
Dosage and Administration:
Colorectal cancer combination regimen 1: ZINOTECAN 125 mg/m2 intravenous infusion over 90 minutes on days 1, 8,15, 22 with LV
20 mg/m2 intravenous bolus infusion on days 1, 8, 15, 22 followed by 5-FU intravenous bolus infusion on days 1, 8, 15, 22 every 6 weeks.
• Colorectal cancer combination regimen 2: ZINOTECAN 180 mg/m2 intravenous infusion over 90 minutes on days 1, 15, 29 with LV
200 mg/m2 intravenous infusion over 2 hours on days 1, 2, 15, 16, 29, 30 followed by 5-FU 400 mg/m2 intravenous bolus infusion on days 1, 2, 15, 16, 29, 30 and 5-FU 600 mg/m2 intravenous infusion over 22 hours on days 1, 2, 15, 16, 29, 30.
• Colorectal cancer single agent regimen 1: ZINOTECAN 125 mg/m2 intravenous infusion over 90 minutes on days 1, 8, 15, 22 then 2-week rest.
• Colorectal cancer single agent regimen 2: ZINOTECAN 350 mg/m2 intravenous infusion over 90 minutes on day 1 every 3 weeks.
Cold Storage: no
A light yellow coloured solution, free from visible particles solution. Irinotecan is used alone or in combination with other medications to treat colon or rectal cancer (cancer that begins in the large intestine). Irinotecan is in a class of antineoplastic medications. It works by stopping the growth of cancer cells. The Molecular formula of Irinotecan Hydrochloride is C33H38N4O6.HCl.3H2O, molecular weight is 677.18 g/mol. The structural formula is:

ZINOTECAN Injection is indicated as a component of first-line therapy in combination with 5-fluorouracil and leucovorin for patients with metastatic carcinoma of the colon or rectum. Irinotecan is also indicated for patients with metastatic carcinoma of the colon or rectum whose disease has recurred or progressed following initial fluorouracil-based therapy.
Patients should be carefully monitored for toxicity and doses of Irinotecan should be modified as necessary to accommodate individual patient tolerance to treatment. Recommended Dose Modifications for Single-Agent Schedules. All dose modifications should be based on the worst preceding toxicity.
A new cycle of therapy should not begin until the toxicity has recovered to NCI grade 1 or less. Treatment may be delayed 1 to 2 weeks to allow for recovery from treatment- related toxicity. If the patient has not recovered, consideration should be given to discontinuing this combination therapy. Provided intolerable toxicity does not develop, treatment with additional cycles of Irinotecan may be continued indefinitely as long as patients continue to experience clinical benefit.
Dosage in Patients with Reduced UGT1A1 Activity
When administered in combination with other agents, or as a single-agent, a reduction in the starting dose by at least one level of Irinotecan should be considered for patients known to be homozygous for the UGT1A1*28 allele . However, the precise dose reduction in this patient population is not known and subsequent dose modifications should be considered based on individual patient tolerance to treatment.
- Read the label carefully before use
- Keep out of the reach of children
ZINOTECAN Injection is administered by intravenous infusion. Care should be taken to avoid extravasation, and the infusion site should be monitored for signs of inflammation. Should extravasation occur, flushing the site with sterile water and applications of ice are recommended.
Premedication with Antiemetics :Irinotecan is emetigenic. It is recommended that patients receive premedication with antiemetic agents. In clinical studies of the weekly dosage schedule, the majority of patients received 10 mg of dexamethasone given in conjunction with another type of antiemetic agent, such as a 5-HT3 blocker (e.g., ondansetron or granisetron). Antiemetic agents should be given on the day of treatment, starting at least 30 minutes before administration of Irinotecan. Physicians should also consider providing patients with an antiemetic regimen (e.g., prochlorperazine) for subsequent use as needed.
Treatment of Cholinergic Symptoms :Prophylactic or therapeutic administration of 0.25 to 1 mg of intravenous or subcutaneous atropine should be considered (unless clinically contraindicated) in patients experiencing rhinitis, increased salivation, miosis, lacrimation, diaphoresis, flushing, abdominal cramping, or diarrhea (occurring during or shortly after infusion of Irinotecan). These symptoms are expected to occur more frequently with higher irinotecan doses.
Immunosuppressant Effects/Increased Susceptibility to Infections :Administration of live or live-attenuated vaccines in patients immunocompromised by chemotherapeutic agents including Irinotecan, may result in serious or fatal infections. Avoid vaccination with a live vaccine in patients receiving irinotecan. Killed or inactivated vaccines may be administered; however, the response to such vaccines may be diminished.
Patients at Particular Risk : In patients receiving either irinotecan/5-FU/LV or 5-FU/LV in the clinical trials, higher rates of hospitalization, neutropenic fever, thromboembolism, first-cycle treatment discontinuation, and early deaths were observed in patients with a baseline performance status of 2 than in patients with a baseline performance status of 0 or 1. Patients who had previously received pelvic/abdominal radiation and elderly patients with comorbid conditions should be closely monitored.
The use of Irinotecan in patients with significant hepatic dysfunction has not been established. In clinical trials of either dosing schedule, irinotecan was not administered to patients with serum bilirubin >2.0 mg/dL, or transaminase >3 times the upper limit of normal if no liver metastasis, or transaminase >5 times the upper limit of normal with liver metastasis. In clinical trials of the weekly dosage schedule, patients with modestly elevated baseline serum total bilirubin levels (1.0 to 2.0 mg/dL) had a significantly greater likelihood of experiencing first-cycle, grade 3 or 4 neutropenia than those with bilirubin levels that were less than 1.0 mg/dL (50% [19/38] versus 18% [47/226]; p<0.001). Patients with deficient glucuronidation of bilirubin, such as those with Gilbert’s syndrome, may be at greater risk of myelosuppression when receiving therapy with Irinotecan.
Ketoconazole, enzyme-inducing anticonvulsants and St. John’s Wort are known to have drug-drug interactions with irinotecan therapy.
Irinotecan commonly causes neutropenia, leucopenia, and anemia, any of which may be severe and therefore should not be used in patients with severe bone marrow failure. Patients must not be treated with irinotecan until resolution of the bowel obstruction. Patients with hereditary fructose intolerance should not be given Irinotecan, as this product contains sorbitol.
Information for Patients : Patients and patients’ caregivers should be informed of the expected toxic effects of Irinotecan, particularly of its gastrointestinal complications, such as nausea, vomiting, abdominal cramping, diarrhea, and infection. Each patient should be instructed to have loperamide readily available and to begin treatment for late diarrhea (generally occurring more than 24 hours after administration of Irinotecan) at the first episode of poorly formed or loose stools or the earliest onset of bowel movements more frequent than normally expected for the patient. One dosage regimen for loperamide used in clinical trials consisted of the following (Note: This dosage regimen exceeds the usual dosage recommendations for loperamide.): 4 mg at the first onset of late diarrhea and then 2 mg every 2 hours until the patient is diarrhea-free for at least 12 hours. Loperamide is not recommended to be used for more than 48 consecutive hours at these doses, because of the risk of paralytic ileus. During the night, the patient may take 4 mg of loperamide every 4 hours. Premedication with loperamide is not recommended. The use of drugs with laxative properties should be avoided because of the potential for exacerbation of diarrhea. Patients should be advised to contact their physician to discuss any laxative use.
Patients should be instructed to contact their physician or nurse if any of the following occur: diarrhea for the first time during treatment; black or bloody stools; symptoms of dehydration such as lightheadedness, dizziness, or faintness; inability to take fluids by mouth due to nausea or vomiting; inability to get diarrhea under control within 24 hours; or fever or evidence of infection.
Patients should be warned about the potential for dizziness or visual disturbances which may occur within 24 hours following the administration of Irinotecan, and advised not to drive or operate machinery if these symptoms occur.
Patients should be alerted to the possibility of alopecia.
Laboratory Tests : Careful monitoring of the white blood cell count with differential, hemoglobin, and platelet count is recommended before each dose of Irinotecan.
UGT1A1 Testing : A laboratory test is available to determine the UGT1A1 status of patients. Testing can detect the UGT1A1 6/6, 6/7 and 7/7 genotypes